Updated February 7, 2023
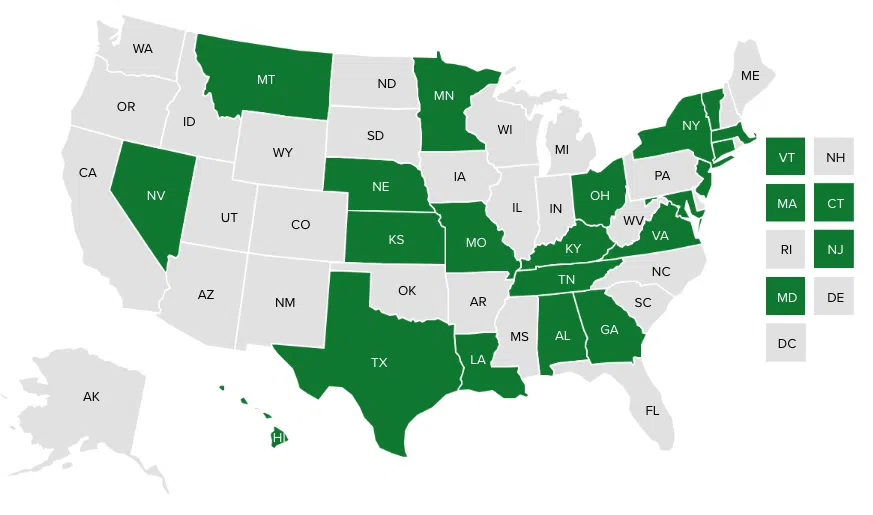
To address high hospital prices, some state health purchasers are using reimbursement rates paid by Medicare as a reference-point to inform their programs’ hospital payments. Through these Reference-Based Pricing to Medicare (RBP) initiatives, state purchasers are seeking to set their reimbursements to more accurately reflect the cost of providing services, rather than negotiating from the much higher hospital chargemaster rates. To date, each state program is establishing its payment as a multiple of the Medicare rate, so the provider will continue to receive a rate higher than that paid by Medicare. Additionally, programs are using RBP to inform the cost of the service but are not necessarily adopting Medicare’s fee-for-service approach. State programs continue to use value-based purchasing arrangements and other payment methodologies. This chart provides a snapshot of state RBP efforts.
States can use the National Academy for State Health Policy (NASHP)’s Hospital Cost Tool to help pursue Reference-Based Pricing to Medicare.
Along with other data important for understanding a hospital’s costs, the tool calculates the commercial rate (as a multiple of Medicare) a hospital can be paid and still breakeven, which is the point at which its revenue equals expense.