Updated September 2020
Note: This resource is no longer being updated. For the most up-to-date information about state approaches to Medicaid managed care (MMC) for children and youth with special health care needs (CYSHCN), check out our new tracker.
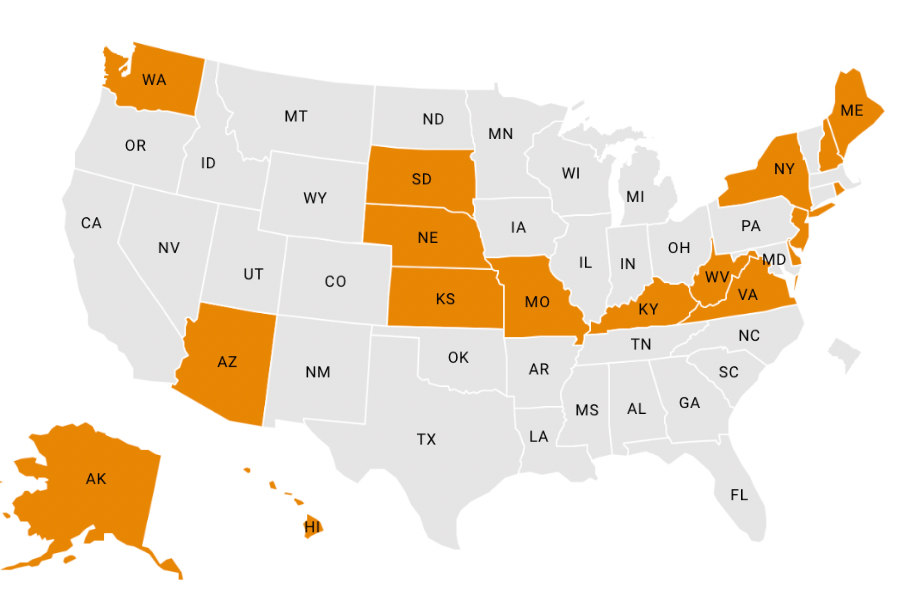
State Medicaid agencies are increasingly providing services to CYSHCN through MMC delivery systems. The two maps on this page and the accompanying chart highlight key characteristics of states’ MMC programs that serve CYSHCN. Additionally, this blog, States Are Increasing their Use of Medicaid Managed Care for Children and Youth with Special Health Care Needs, identifies trends in the design of these programs since NASHP’s last analysis in 2017.