Most states deliver Medicaid behavioral health services through contracts with managed care organizations (MCO). Federal regulation requires that these contracts include network adequacy standards for specified provider types, including behavioral health providers. When developing network adequacy standards, states must consider anticipated Medicaid enrollment and service utilization; the volume and types of providers needed; the distance and travel time between network providers and Medicaid enrollees; and the physical accessibility of services, including through telemedicine.
Including these network adequacy requirements in managed care contracts helps states to ensure that all plan members have access to behavioral health care providers. In addition to a robust network of providers, states are also taking opportunities to enhance and build out access via telehealth. In rural and frontier areas, where networks can be more challenging to develop, this can be particularly helpful.
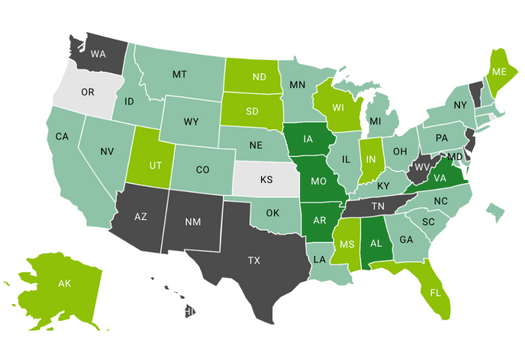
This map, with links to available MCO contracts and requests for applications (RFA), demonstrates how Medicaid managed care states are using contractual language to increase access to behavioral health services, improve behavioral health provider networks, and leverage telehealth to support access to care.