While state policymakers across the country grapple with oral health care access challenges, California, Pennsylvania, and Connecticut are incentivizing their Medicaid plans and providers to deliver pediatric oral health services in innovative ways, with a special focus on community-based solutions.
- Under its Medicaid section 1115 waiver, California incentivizes dental care coordination by community health workers and the use of telehealth.
- Pennsylvania has a number of Medicaid managed care strategies in place to foster innovation, including making dollars available to managed care organizations (MCOs) to engage public health dental hygiene practitioners.
- Connecticut similarly includes oral health in its statewide Medicaid payment and delivery reform.
Through these incentives and performance measures, explored below, Medicaid agencies are supporting workforce innovations to address children’s oral health.
The Case for Oral Health Workforce Innovation in Medicaid
Dental decay is preventable, yet it is the most common chronic condition among children.[1] Because oral health and overall health are interconnected, unmet oral health needs can negatively affect overall health by making chewing difficult, leading to lost school days, and damaging self-esteem.[2],[3],[4] Inability to access dental care can be fatal – in 2007 Deamonte Driver, a 12-year-old boy enrolled in Medicaid, died after an untreated tooth infection spread to his brain.
Medicaid is a key lever in addressing oral health care needs, particularly for children, because the Early, Periodic, Screening, Diagnostic and Treatment (EPSDT) benefit requires dental coverage for children and adolescents. The Centers for Medicare & Medicaid Services (CMS) encourages state Medicaid agencies to increase children’s access to dental services through Medicaid and the Children’s Health Insurance Program (CHIP).[5] The Child Core Set of measures that Medicaid agencies can report to CMS includes dental and oral health. The 2011 CMS Oral Health Strategy outlines options for state Medicaid agencies to increase children’s access to care, including workforce strategies, such as provider outreach and recruitment, and reimbursement for services provided by additional types of providers to deliver preventive services.
Workforce strategies are critical to address children’s oral health needs in part because oral health care provider shortages persist across the country. Health Professional Shortage Areas (HSPAs) for dental care exist in 49 states.[6] Rural communities have significantly fewer oral health providers than urban communities and therefore less access to services.[7] To offset shortages, states are introducing new provider types or expanding the services existing providers can deliver. Dentists and dental hygienists (working independently or under dentist or physician supervision) practice in every state. Pediatricians and other primary care medical providers deliver preventive oral health services and refer children to dentists.[8] In 10 states, dental therapists can provide preventive and restorative care.[9] Five states have introduced legislation for advanced dental hygiene practitioners, and 21 states allow community dental health coordinators to assist in community-based care coordination and prevention outreach.[10],[11]
To address children’s oral health needs and access to care, Medicaid officials in California, Pennsylvania, and Connecticut use payment and performance-based strategies to engage the providers authorized to deliver oral health services in their states in the continuum of care.
California’s Dental Transformation Initiative
California’s current 1115 waiver focuses on transforming health care service delivery and quality for Medicaid (Medi-Cal) members, and it includes the Dental Transformation Initiative (DTI). The DTI aims to increase pediatric preventive dental service utilization, diagnose early childhood caries[12] through caries risk assessment (CRA) and disease management, and continuity of care for children enrolled in Medicaid. The DTI budget is up to $740 million over five years (through 2020) for provider incentive payments in four domains: pediatric preventive dental service utilization, caries risk assessment and disease management, continuity of care, and local dental pilot programs (LDPPs).
DTI incentives include:
- Semi-annual payments to dental service office locations or safety net clinics that provide preventive services to more children;
- Payments to dentists for performing pre-identified treatment plans for children ages 6 and younger (where treatment plans include CRA with motivational interviewing, nutritional counseling, and antimicrobials; fluoride varnish application; toothbrush prophylaxis; exams; and increased frequency of services depending on risk level);
- Annual, tiered payments to dental service office locations that provide exams to an enrolled child (up to age 20) for continuous years (e.g., tier one payments are provided on a per-child basis for those with two or more exams from the same service location for two consecutive years); and
- Payments specific to each LDPP program.
The LDPPs use innovative strategies to address the primary DTI aims of pediatric preventive dental service utilization, risk assessment and disease management, and/or continuity of care. Community organizations submitted applications for LDPPs, and as of July 2019, the state Medicaid agency had contracts with 13 LDPPs. Many LDPPs employ workforce strategies such as telehealth and care coordination or case management to meet the DTI goals.[13]
- Five LDPPs are piloting a virtual dental home (VDH)[14] – in this system children receive preventive and other oral health services in community settings, such as schools. Dental hygienists and assistants with special training collect information and provide preventive services. Using technology, dentists in a different physical location review the information and may direct provision of additional services. The VDH also connects children with complex dental needs to a local dentist. The VDH model began at The Pacific Center for Special Care at the University of the Pacific Arthur A. Dugoni School of Dentistry. A Health Resources and Services Administration (HRSA) State Oral Health Workforce Grant to the California Department of Public Health enabled expansion of the VDH to additional sites.[15],[16]
- The Sonoma County LDPP (“Cavity Free Sonoma”) is training and integrating community dental health workers (CDHWs) into dental teams at seven federally qualified health centers (FQHCs) to decrease dental disease among Medicaid-eligible children ages six and younger. The CDHWs provide culturally appropriate oral health information to caregivers and children, assist with caries risk assessment, track patient data, and provide dental case management. CDHWs help caregivers navigate medical and social service systems, and they follow up with caregivers to ensure children complete appointments.
A number of state policies underpin and support the DTI. The VDH was initially tested under the state’s Health Workforce Pilot Projects Program, which allows organizations to test or evaluate new or expanded provider roles before changing licensing laws. Based on the VDH results, the state made scope-of-practice changes for dental hygienists and dental assistants, amended the state Medicaid plan to allow allied dental professional enrollment and billing, and to cover the technology used in VDH. These changes facilitated additional VDH piloting and implementation.
Additionally, the state legislature directed a portion of state tobacco tax revenue to be used for supplemental payments to dentists for certain services, and a $30 million loan repayment program for dentists who commit to serve Medicaid patients for five or ten years.[17] (The American Dental Education Association maintains a list of loan repayment programs by state). Dentists in California can receive up to $300,000 through the loan repayment program, and awardees must agree to ensure Medicaid beneficiaries comprise 30 percent of their patient caseload. In July 2019, the Medicaid agency announced $10.5 million in loan repayment awards to 40 dentists.
The Medicaid agency and public health department collaborate through these efforts and the statewide oral health plan,[18] which complements and references the DTI. As part of the oral health plan, California aims to support community-clinical linkages by maximizing the use of trained personnel, such as community health workers and public health nurses, as well as co-locating medical and dental providers.[19]
DTI results to date indicate improvement. The statewide pediatric preventive service utilization rate increased 7.48 percentage points from 2014 to 2017, and continuity of care increased 2.6 percentage points from 2015 to 2017.[20]
Pennsylvania’s Medicaid Managed Care Strategies
Pennsylvania also encourages MCOs and providers to increase access to dental care for children in a number of ways that promote workforce innovation. Two specific strategies are performance-based incentives and allocating a portion of MCOs’ capitated payments to initiatives that focus on community-based care management, including for oral health.
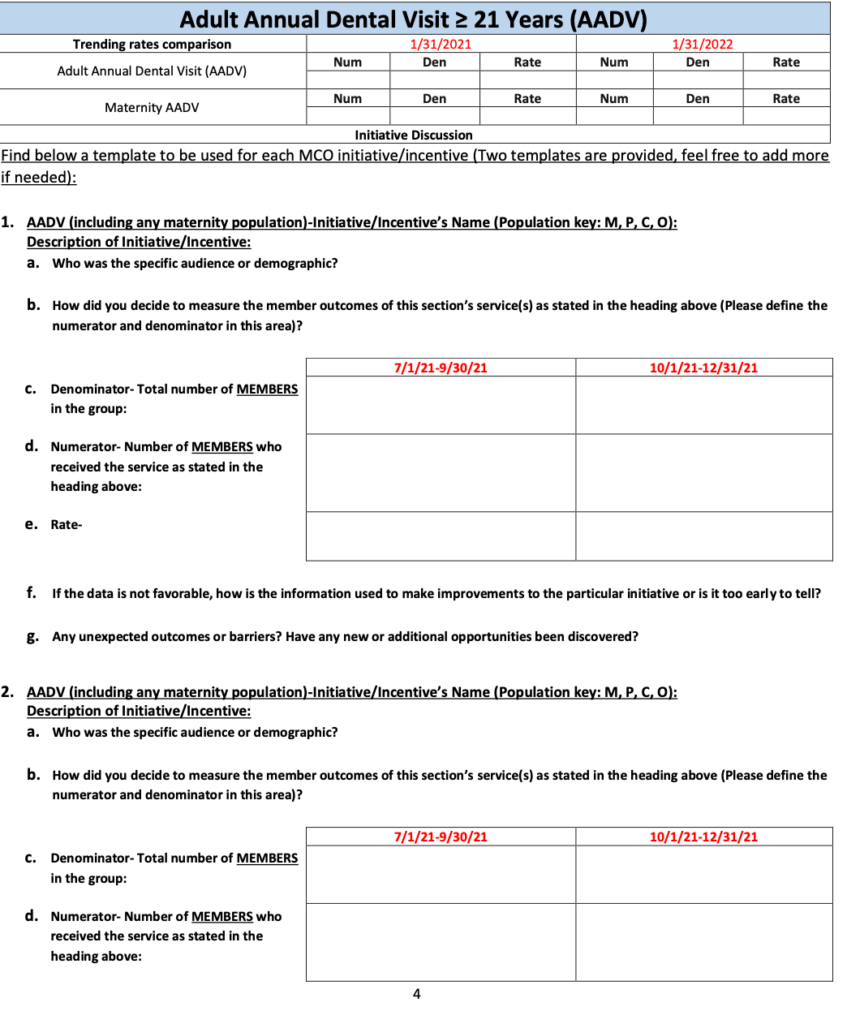
Pennsylvania has a carved-in (or comprehensive managed care) Medicaid dental delivery system in which MCOs (physical health – PH – MCOs in the state) are responsible for medical and dental services. The state has an MCO and provider dental pay-for-performance (P4P) measure with related performance improvement projects (PIPs) to improve access to pediatric oral health services.[21]
The measure is annual dental visit for youth ages 2 to 20. The PH-MCO receives an incentive payment for meeting the state benchmark and an incremental improvement compared to past performance on the measure. PH-MCOs are eligible to earn a double payout for meeting certain benchmarks or being responsible for a double offset if they do not meet those benchmarks. PH-MCOs also must include an incentive for the dentist as part of provider P4P for the measure. The dental P4P consists of two age bands, 0-5 years and 6-20 years. There is an emphasis placed on the lower age band and children who have not received a preventive dental service within the previous calendar year in order to increase education and obtaining early preventive dental care.
To improve access, some PH-MCOs offer incentives to pediatricians who make dental referrals for children who then receive a dental service (as evidenced by a dental claim). Some PH-MCOs partner with FQHCs to improve access by supporting co-location of primary medical and dental care. Examples of other innovative plan efforts to increase access include the use of a mobile dental unit with pediatric dental providers and the implementation of a small dental home pilot project.
What services can Pennsylvania’s Public Health Dental Hygiene Practitioners (PHDHPs) provide?
In Pennsylvania, a registered dental hygienist can be certified as a PHDHP to provide dental hygiene services without dentist supervision in specific public health practice sites, such as schools, correctional facilities, health care facilities, and FQHCs. PHDHPs can clean teeth, take X-rays, polish fillings, identify cavities, evaluate patients, and provide oral health education to patients without dentist supervision.
The P4P dental measure and related dental PIPs have been successful. From 2016 to 2018, annual dental visit rates increased by 3.09 absolute percentage points, making the annual dental visit rate 63 percent statewide. Every Pennsylvania plan is currently above the 50 percent national benchmark, and while there is still room for improvement, each plan has improved since the inception of these projects. The state will continue to monitor progress in these areas and especially look at demographics and oversight of the managed care program. A specific area of focus is examining racial/ethnic or geographic disparities in dental care.
Another managed care strategy in Pennsylvania is the availability of Community-Based Care Management (CBCM) dollars for PH-MCOs to implement innovative initiatives that increase access to oral health services. CBCM dollars must be used for community-based projects, either for staffing or for the initiatives themselves. With this funding, PH-MCOs have embedded registered nurses or community health workers (CHWs) in care settings, helped enrollees with transportation to appointments, and conducted public education. Some PH-MCOs use CBCM dollars for oral health services, including mobile dental vehicles, and working with public health dental hygiene practitioner (PHDHP) initiatives. MCOs can enroll PHDHPs, and CBCM guidance specifically requires PHDHP initiatives. In this way, CBCM dollars assist plans in meeting P4P benchmarks and PIP goals.
An Emerging Model: Connecticut’s Oral Health Focus in Medicaid Payment and Delivery Reform
Connecticut’s State Innovation Model (SIM) initiative aims to improve overall community health, access to and quality of care, and health equity through payment and delivery reform. One component of SIM, the Community and Clinical Integration Program (CCIP), provides technical assistance to help provider organizations and FQHCs improve primary care delivery and patient outcomes.[22] CCIP has three core standards: comprehensive care management, health equity improvement, and behavioral health integration, as well as three elective standards, one of which is oral health. This standard includes screening for oral health risk factors and symptoms, developing treatment plans, providing treatment, and tracking oral health outcomes and improvement over time. Although implementation is in the early stages, one participating FQHC has chosen this oral health elective standard. Connecticut recognizes the importance of oral health as it relates to overall health and this awareness will be a consideration in any future practice transformation and payment reform efforts.
Considerations and Conclusion
Some lessons from these state efforts to promote pediatric oral health care access through workforce innovation include:
- Engage the dental community. States with comprehensive managed care can elevate dental care within MCOs, for example, by requiring each plan to have a dental director. Pennsylvania has seen increased dental provider engagement since implementing this change.
- Consider pilot programs. Pilot programs offer the opportunity to start small, build buy-in, and receive early input. They also can help states determine possible impact and address challenges on a small scale before rolling out statewide.
- Leverage multiple funding streams, when possible, and consider a multi-pronged approach for oral health workforce innovation. California has leveraged tobacco tax revenue and federal grants to support innovations across Medicaid and public health, and with an academic partner.
- Consider the unique needs of FQHCs and safety net providers. FQHCs often can lead the way in co-location of dental and overall health services and providers, but some safety net facilities/organizations establish contracts for dental care with the private sector. Additionally, due to federal law, FQHCs bill Medicaid agencies for services differently than other providers.[23] These realities can create challenges tracking utilization or other data. A contractor and a dental consultant have provided assistance engaging and supporting safety net providers who opt in to participate in the California DTI.
Dental decay is preventable, yet unmet oral health needs persist. Payment and quality measurement policies in California, Connecticut, and Pennsylvania demonstrate how Medicaid agencies – often in collaboration with public health agencies – can promote oral health workforce innovation to help Medicaid-eligible children access needed dental and oral health care. While states often face financial and data barriers, emerging efforts to engage providers, such as community dental health workers, or dental hygienists and assistants, with advanced training, and to leverage telehealth show promise.
Notes
[1] Centers for Disease Control and Prevention. “Dental Caries (Tooth Decay).” Hygiene-related Diseases. September 22, 2016. https://www.cdc.gov/healthywater/hygiene/disease/dental_caries.html.
[2] Jackson, Stephanie L., William F. Vann, Jonathan B. Kotch, Bhavna T. Pahel, and Jessica Y. Lee. “Impact of Poor Oral Health on Children’s School Attendance and Performance.” American Journal of Public Health 101, no. 10 (2011): 1900-906. doi:10.2105/ajph.2010.200915. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222359/
[3] Kelekar, Uma, and Shillpa Naavaal. “Hours Lost to Planned and Unplanned Dental Visits Among US Adults.” Preventing Chronic Disease 15 (2018). doi:10.5888/pcd15.170225.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5772383/
[4] Health Policy Institute, American Dental Association. “Oral Health and Well-Being in the United States.” https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/OralHealthWell-Being-StateFacts/US-Oral-Health-Well-Being.pdf?la=en.
[5] CMS recently completed the Medicaid Innovation Accelerator Program Children’s Oral Health Initiative Value-Based Payment Technical Support Opportunity for states focused on selecting, designing, and testing a value-based payment approach to improve children’s oral health outcomes. See https://www.medicaid.gov/state-resource-center/innovation-accelerator-program/iap-functional-areas/value-based-payment/index.html
[6] National and State-level Projections of Dentists and Dental Hygienists in the U.S.: 2012-2025. Washington, D.C.: U.S. Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce, National Center for Health Workforce Information and Analysis, 2015. https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/projections/nationalstatelevelprojectionsdentists.pdf
[7] National Advisory Committee on Rural Health and Human Services, Improving Oral Health Care Services in Rural America: Policy Brief and Recommendations. December 2018. https://www.hrsa.gov/sites/default/files/hrsa/advisory-committees/rural/publications/2018-Oral-Health-Policy-Brief.pdf
[8] For example, see: Centers for Medicare and Medicaid Services. “Keep Kids Smiling: Promoting Oral Health Through the Medicaid Benefit for Children & Adolescents.” September 2013. https://www.medicaid.gov/medicaid/benefits/downloads/keep-kids-smiling.pdf; Cantrell, Chris. “Engaging Primary Care Medical Providers in Children’s Oral Health” (National Academy for State Health Policy, 2009). https://www.nashp.org/engaging-primary-care-medical-providers-childrens-oral-health/.
[9] “New Mexico’s Passage of Dental Therapy Law Builds National Momentum for Changing Provision of Dental Care Amid Oral Health Crisis.” Community Catalyst. March 29, 2019. https://www.communitycatalyst.org/news/press-releases/new-mexicos-passage-of-dental-therapy-law-builds-national-momentum-for-changing-provision-of-dental-care-amid-oral-health-crisis.
[10] American Dental Hygienists’ Association. “The Benefits of Dental Hygiene-Based Oral Health Provider Models.” April 2016. https://www.adha.org/resources-docs/75112_Hygiene_Based_Workforce_Models.pdf.
[11] American Dental Association. “Solutions: About CDHCs.” Action for Dental Health. https://www.ada.org/en/public-programs/action-for-dental-health/community-dental-health-coordinators.
[12] Early childhood caries is the presence of one or more decayed, missing, or filled tooth surfaces in a primary tooth in children younger than six years of age. See American Academy of Pediatric Dentistry, “Definition of Early Childhood Caries” https://www.aapd.org/assets/1/7/D_ECC.pdf
[13] California Department of Health Care Services, “Medi-Cal 2020 Waiver Dental Transformation Initiative, Domain 4 Summary of Local Dental Pilot Program Applications,” March 8, 2018. https://www.dhcs.ca.gov/provgovpart/Documents/DTI/Domain%204/Medi-Cal_2020_DTI_D4_LDPP_Summary_030818.pdf
[14] University of the Pacific, Arthur A. Dugoni School of Dentistry. “About Virtual Dental Home” https://dental.pacific.edu/departments-and-groups/pacific-center-for-special-care/innovations-center/virtual-dental-home-system-of-care
[15] University of the Pacific, Arthur A. Dugoni School of Dentistry. “Pacific Center Receives More than $3.5 Million in New Grants for Virtual Dental Home Projects,” October 13, 2017.
[16]California Department of Public Health Office of Oral Health. “Oral Health Program Projects.” https://www.cdph.ca.gov/Programs/CCDPHP/DCDIC/CDCB/Pages/OralHealthProgram/OralHealthProjects.aspx
[17] See www.CalHealthCares.org to learn more about loan repayment program eligibility and requirements.
[18] California Department of Public Health Office of Oral Health, Statewide Oral Health Plan 2018-2028, January 2018. https://www.cdph.ca.gov/Documents/California%20Oral%20Health%20Plan%202018%20FINAL%201%205%202018.pdf
[19] Kumar, Jayanth. “Public Health and Dental Care Collaboration in California.” Webinar presentation for the National Academy for State Health Policy. July 30, 2019.
[20] Jackson, Alani. “California Oral Health Innovations.” Webinar presentation for the National Academy for State Health Policy. July 30, 2019.
[21] To learn more about relevant PIPs, see Medicaid Oral Health Performance Improvement Projects: A How-To-Manual for States. Centers for Medicare & Medicaid Services Oral Health Initiative, 2015. https://www.medicaid.gov/medicaid/benefits/downloads/pip-manual-for-states.pdf
[22] Connecticut State Innovation Model (SIM) Report of the Practice Transformation Taskforce on Community and Clinical Integration Program Standards for Advanced Networks and Federally Qualified Health Centers. Core Elective Standards. CT.gov, 2016. https://portal.ct.gov/-/media/OHS/SIM/PracticeTransformationTaskForce/CCIP-Reports-and-Publications/ccip_report_standards_updated_12_30_16.pdf?la=en
[23] To learn more, see for example, Medicaid and CHIP Payment and Access Commission. Medicaid Payment Policy for Federally Qualified Health Centers, December 2017. https://www.macpac.gov/publication/medicaid-payment-policy-for-federally-qualified-health-centers/
Acknowledgements
The authors wish to thank the state officials in California, Connecticut, and Pennsylvania who graciously shared their experiences and reviewed a draft of this publication. Trish Riley, Kitty Purington, and Elinor Higgins of NASHP provided helpful guidance or assistance. Finally, we thank the Health Resources and Services Administration (HRSA) officials who provided thoughtful input.
This project was supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) under grant number UD3OA22891, National Organizations of State and Local Officials. This information or content and conclusions are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the US government.